What is being changed
Cornea reshaping, lens replacement, fluid management in the retina, pressure control in glaucoma. If you cannot describe the “mechanical” change, you are vulnerable to hype.
What the procedure changes, what it treats, what the tradeoffs are, and what recovery typically involves.
Procedures tend to sound simple in marketing copy. The useful version includes candidacy, alternatives, measurable outcomes, and the realistic list of risks and recovery constraints.
Most eye procedures fall into a small number of categories: refractive procedures that change how the eye focuses, lens procedures that replace or modify the natural lens, retina procedures that treat macular and vascular disease, and surface procedures that address corneal and ocular surface problems. Each category has different goals and different definitions of success. Some are elective and lifestyle oriented. Others are disease management where delay can matter.
A procedure is a tool. The right tool depends on goals, anatomy, and risk tolerance.
A useful way to evaluate any eye procedure is to separate: the underlying problem (diagnosis), the functional goal (what you want to be able to do), and the acceptable tradeoffs (night vision, dry eye risk, reading glasses dependence, recovery time). Many disagreements between patients and clinicians come from mismatched goals rather than disagreement about facts.
Cornea reshaping, lens replacement, fluid management in the retina, pressure control in glaucoma. If you cannot describe the “mechanical” change, you are vulnerable to hype.
“20/20” is not the only outcome. Contrast, glare, halos, stability over time, and reading vision all matter. Some procedures optimize one metric while sacrificing another.
Glasses, contacts, drops, monitoring, or different procedures. “No procedure” can be the best option when risk outweighs benefit or when timing is not right.
If you are navigating scheduling, referrals, insurance, or second opinions, see Care Guide.
Lens replacement that restores clarity, often with choices about glasses dependence.
Cataract surgery replaces the eye’s natural lens with an artificial intraocular lens (IOL). The central goal is restoring clarity and functional vision when lens aging reduces contrast and increases glare. In modern practice, cataract surgery also includes decisions about refractive goals, such as whether you prefer better distance vision without glasses, better near vision, or a blended option.
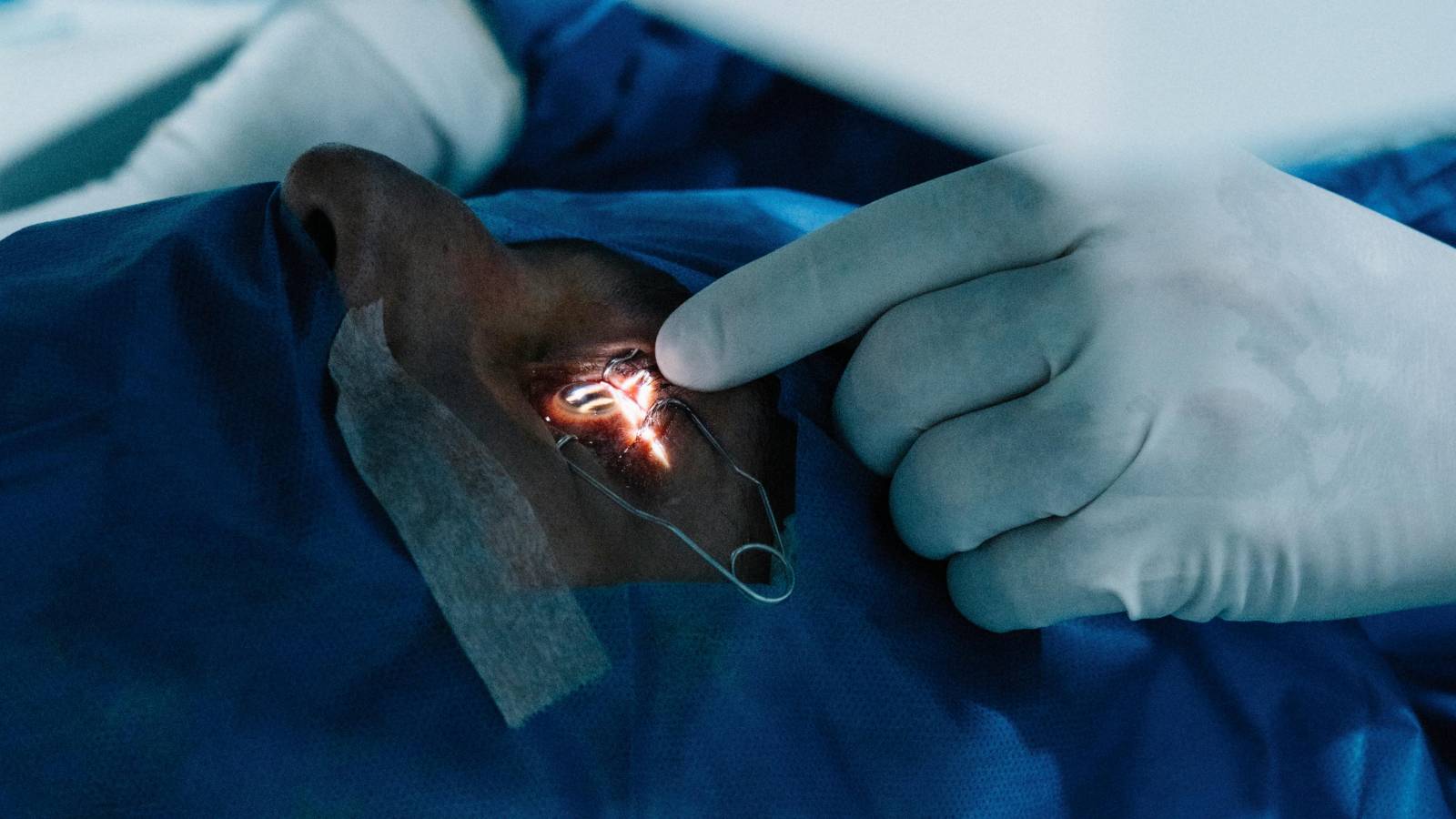
Monofocal lenses often prioritize one distance. Multifocal or extended depth lenses can reduce reading glasses dependence for some people, but they can increase glare or halos in some settings. Toric lenses address astigmatism.
Many people feel improvement quickly, but vision can fluctuate during healing. Drops, activity restrictions, and follow up visits are part of the process.
Refractive surgery that reshapes the cornea, with candidacy being the main filter.
LASIK and PRK are refractive procedures that reshape the cornea to change how light focuses. They are often discussed as a “freedom from glasses” story, but candidacy and ocular surface health determine outcomes. Dry eye tendency, corneal thickness, corneal shape regularity, and prescription stability are common factors in screening.

Digital comfort matters here because surface symptoms can be amplified after refractive procedures, especially in people with pre existing dryness. See Digital Life and Habits for baseline drivers.
Injections, lasers, and surgery, usually for disease management rather than comfort.
Retina treatments are often used for macular disease, diabetic retinopathy, and retinal vascular problems. Many modern protocols include anti VEGF injections (commonly called “retina injections”) that reduce abnormal blood vessel activity and leakage in certain conditions. Laser can be used in specific scenarios, and retinal surgery is used for problems like retinal detachment and some macular interface disorders.

Abnormal vessel growth and leakage in certain macular conditions. The goal is often preserving function and preventing worsening, not creating perfect vision.
Many protocols are schedule dependent. Skipping follow up can reduce effectiveness, even when symptoms seem stable.
Diabetes and vascular risk factors show up strongly in retina outcomes. See Nutrition for the long view on risk.
Drops are common, but laser and surgical options exist, including MIGS.
Glaucoma management aims to reduce the risk of optic nerve damage progression, often by lowering intraocular pressure. Drops are common, but laser procedures and surgeries are also used. Newer approaches include minimally invasive glaucoma surgery (MIGS) devices that can be combined with cataract surgery in selected patients.
The key thing to understand is that glaucoma treatment is usually about long term risk reduction. Many patients feel normal throughout early disease, so monitoring and adherence are often more important than symptom relief.
From dry eye treatments to corneal transplants, the scope is wide.
Surface procedures can range from in office treatments for meibomian gland dysfunction to surgical procedures for corneal disease. The ocular surface is sensitive, so outcomes depend heavily on baseline surface health, environment, and consistent follow up. Some treatments aim for symptom control, while others are structural and vision restoring.
If your main complaint is burning, fluctuating blur, or screen intolerance, you may be in the surface category even if your “vision” measures well. The most useful first step is often a good evaluation of tear film stability and eyelid margin health.
These help convert a sales pitch into a clinical decision.
For practical visit prep, records, and second opinion strategy, see Care Guide.
Short answers with useful context.
No. Procedures are tools with benefits and risks. In many scenarios, conservative options are best until function is limited or disease progression risk changes the equation.
Because anatomy and baseline surface health strongly predict outcomes. Screening is not gatekeeping, it is risk management.
Choosing a procedure based on one metric (like “no glasses”) without defining acceptable tradeoffs for night vision, dryness, reading, and recovery constraints.